“Something’s Off, But I Can’t Explain It”
Have you ever left a family gathering feeling worse than when you arrived, but unsure why?
Do you carry guilt, anxiety, or confusion around your childhood or your relationship with a parent who seems loving in public but cruel in private?
You might be experiencing the lasting effects of narcissistic family abuse a hidden, often misunderstood form of trauma that doesn’t leave physical bruises, but does deep psychological harm.
Backed by diagnostic criteria in the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5th Edition), narcissistic traits in parents or caregivers can shape an entire family system. These dynamics impact your brain, relationships, and self-worth—often for decades.
Understanding Narcissistic Family Abuse (DSM-5-Informed)
Narcissism isn’t just vanity—it’s a pattern of behaviour characterised by:
A lack of empathy
Need for control and admiration
Manipulation of others to meet emotional needs
Refusal to take responsibility for harm
The DSM-5 defines narcissistic personality disorder (NPD) by traits such as:
Grandiosity
Excessive need for admiration
Exploitative interpersonal behaviour
A deep lack of empathy
Sense of entitlement
When a caregiver has these traits, they can destabilise the entire family dynamic—creating conditions for narcissistic family abuse.
How Narcissistic Family Abuse Impacts the Brain
Children in narcissistic homes often live in a state of chronic emotional threat, activating their fight-or-flight response repeatedly.
This can lead to:
Overactive amygdala (fear response)
Impaired hippocampus (memory and emotion regulation)
Underdeveloped prefrontal cortex (decision-making)
“Emotional abuse is as harmful as physical abuse, particularly in childhood, and changes brain development.”
— Teicher et al., Harvard Medical School
This physiological toll is one reason narcissistic family abuse often leads to long-term C-PTSD, anxiety, and emotional dysregulation.
12 Toxic Rules That Drive Narcissistic Family Abuse
(Adapted from Dr. Linda Martinez-Lewi)
-
The narcissist is always right.
Your thoughts and feelings don’t matter if they challenge the narcissist.
-
They are the centre of everything.
Your emotions, milestones—even your pain—are secondary.
-
Truth is dangerous.
You’re punished or silenced for telling it.
-
Your feelings are a threat.
They may be mocked, dismissed, or weaponised.
-
Outshining the narcissist is not allowed.
Success is belittled or stolen.
-
Children are divided into roles.
“Golden child” vs. “scapegoat”—both emotionally damaging.
-
Image over reality.
The family must look perfect, even if it’s falling apart inside.
-
Silence protects survival.
Speaking up leads to emotional retaliation or shame.
-
Boundaries are betrayal.
Privacy, independence, or “no” are punished.
-
Loyalty is demanded.
You’re expected to stay loyal—even at your own expense.
-
Abuse is disguised as love.
Control is framed as care: “I do this for your own good.”
-
The family secret must stay hidden.
You’re discouraged from therapy or speaking out.
Case Study: A Realistic Example of Narcissistic Family Abuse
Jas, 32, grandmother was warm and charming. At home, she was controlling, critical, and emotionally cold.Jas was subtly conditioned to distrust her father, who her mother portrayed as weak and emotionally distant—despite his quiet support. Over time, Jas became estranged from him and isolated from extended family members who questioned her mother’s behaviour.
This is a classic pattern of narcissistic family abuse, where the abuser isolates, divides, and distorts relationships to retain control.
In therapy, Jas began unravelling the narrative. She reconnected with her father, established healthy boundaries with her mother, and started the journey of healing her sense of self—free from shame and manipulation.w up with a narcissistic mother who controlled every emotional current in the household. In public, her
Long-Term Effects of Narcissistic Family Abuse
If you were raised in a narcissistic family system, you may experience:
Over-apologising or people-pleasing
Emotional flashbacks
Anxiety, depression, or low self-worth
Difficulty trusting others
Attracting emotionally unavailable or manipulative partners
Shame or guilt when setting boundaries
This is the legacy of narcissistic family abuse—but it can be healed.
How to Heal After Narcissistic Family Abuse
1. Name the Pattern
Understanding narcissistic dynamics helps lift the fog of shame and self-blame.
2. Reclaim Boundaries
Boundaries are not betrayal—they’re survival. Start small and stay consistent.
3. Seek Trauma-Informed Support
Work with a therapist trained in:
EMDR (Eye Movement Desensitisation and Reprocessing)
IFS (Internal Family Systems)
Schema Therapy
4. Soothe the Nervous System
Use grounding techniques, breathwork, or polyvagal exercises to feel safe in your body again.
5. Rebuild Relationships on Your Terms
Surround yourself with people who see you—not just the version your family allowed.
6. Break the Cycle
You’re allowed to parent differently. You can offer emotional safety that wasn’t given to you.
Support Services
1800RESPECT – National sexual, domestic, and family violence service (📞 1800 737 732)
Blue Knot Foundation – Support for adult survivors of complex childhood trauma (📞 1300 657 380)
Lifeline Australia – 24/7 mental health crisis line (📞 13 11 14)
Further Resources
Adult Children of Emotionally Immature Parents — Lindsay C. Gibson
The Body Keeps the Score — Dr. Bessel van der Kolk
Will I Ever Be Good Enough? — Dr. Karyl McBride
CPTSD: From Surviving to Thriving — Pete Walker
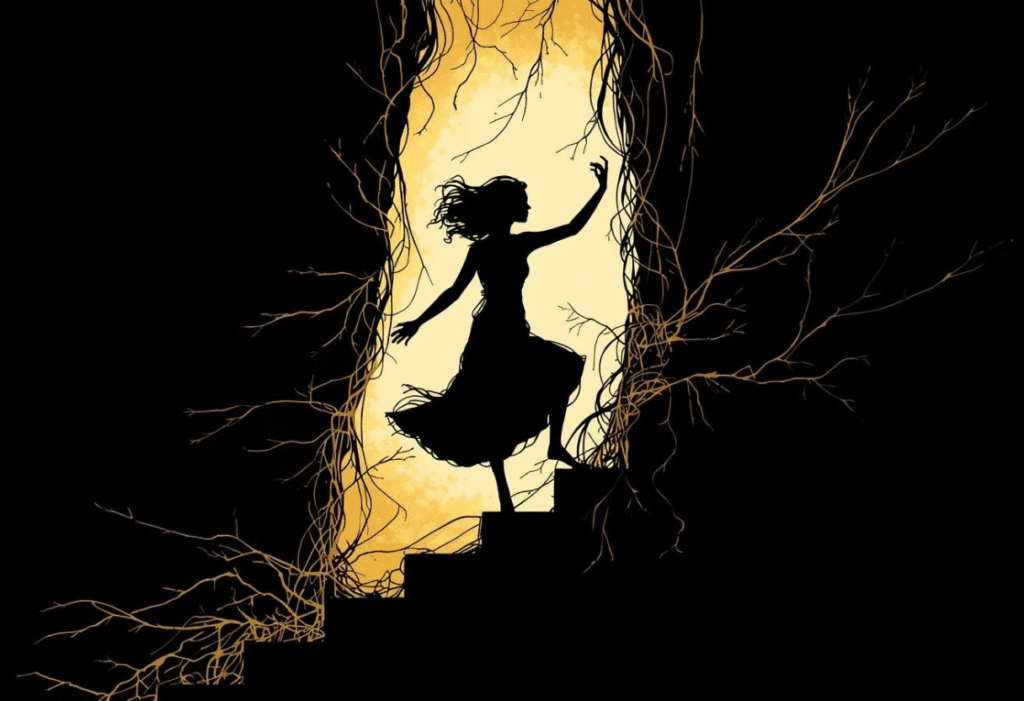
Final Thoughts: “You Are Not What They Told You”
Narcissistic family abuse is subtle but powerful. It shapes your nervous system, your identity, and how you love. But those patterns can be rewritten.
You can:
Reconnect with your truth
Set boundaries that protect your peace
Build relationships grounded in mutual respect and emotional safety
 Visit the Meducate Blog for practical, expert-informed resources for parents, caregivers, and professionals.
Visit the Meducate Blog for practical, expert-informed resources for parents, caregivers, and professionals.






 Visit the
Visit the