Ivermectin’s Leap into Cancer Therapy
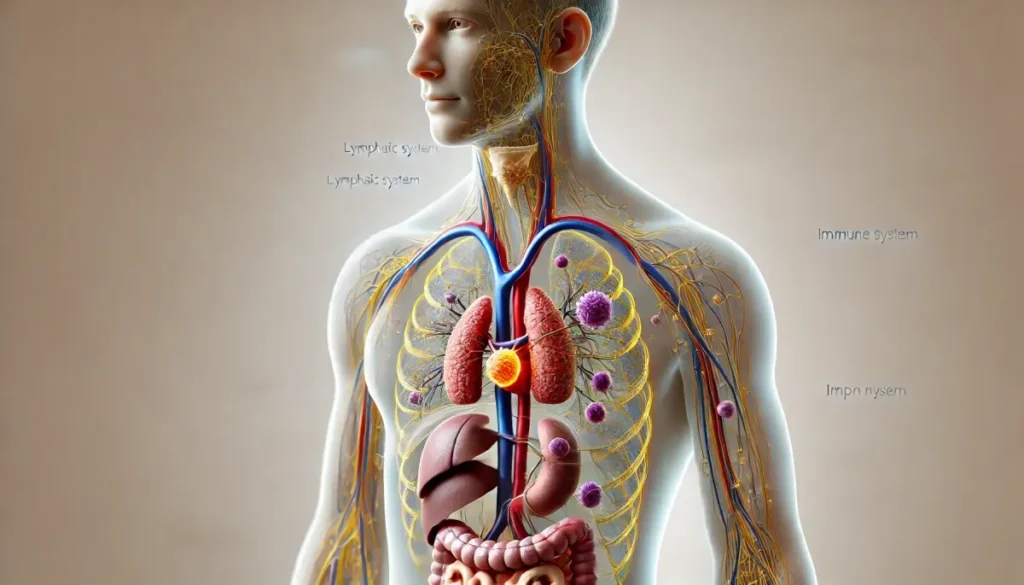
Ivermectin’s anticancer properties reveal a remarkable journey from an anti-parasitic medication to a promising cancer treatment candidate. Scientists have discovered that this versatile drug exhibits significant anti-tumor effects across various cancer cell types through multiple mechanisms.
They have found that ivermectin works by inhibiting cell proliferation, preventing metastasis, and disrupting blood vessel formation in tumours. Research shows that it targets cancer cells through different pathways, including programmed cell death and autophagy, while also showing potential in combating drug resistance when combined with traditional chemotherapy agents.
Key Takeaways:
-
Ivermectin demonstrates anti-tumor properties by inhibiting cancer cell proliferation, metastasis, and angiogenic activity
-
The drug works through PAK1 kinase to regulate multiple signalling pathways in cancer cells
-
It promotes different types of programmed cell death including apoptosis, autophagy, and pyroptosis
-
Ivermectin shows effectiveness against tumour stem cells and helps reverse multi-drug resistance
-
Maximum benefits are achieved when used in combination with other chemotherapy drugs
Fundamental Properties of Ivermectin
To understand ivermectin’s potential as an anticancer agent, one must first examine its fundamental characteristics that make it a versatile compound. The drug belongs to the avermectin family, a group of macrocyclic lactones with exceptional pharmacological properties. These properties include high lipid solubility, allowing for effective distribution throughout the body, and a remarkable safety profile when administered at standard therapeutic doses.
Chemical Structure and Properties
Properties of ivermectin center around its unique chemical structure, consisting of two closely related homologous compounds: 22,23-dihydroavermectin B1a and B1b. The molecule contains a 16-membered macrocyclic lactone ring with specific modifications that enhance its biological activity. Its molecular weight of approximately 875 daltons and high lipophilicity contribute to its excellent tissue penetration and distribution characteristics.
Traditional Anti-parasitic Applications
Beside its emerging role in cancer research, ivermectin has established itself as a cornerstone in anti-parasitic treatment worldwide. The drug demonstrates remarkable efficacy against various parasitic infections, including river blindness (onchocerciasis) and lymphatic filariasis, earning its discoverers the 2015 Nobel Prize in Medicine.
To achieve optimal anti-parasitic effects, ivermectin operates through a specific mechanism involving glutamate-gated chloride channels in parasitic organisms. The drug’s selective toxicity to parasites while maintaining safety in mammals has made it an necessary tool in global health initiatives, with millions of doses administered annually in endemic regions.
Mechanisms of Anticancer Action
Assuming the broad spectrum of ivermectin’s anticancer properties, the drug exhibits multiple mechanisms to combat various types of cancer cells. The compound demonstrates its effectiveness through several pathways, including the inhibition of cell proliferation, reduction of metastatic potential, and suppression of angiogenic activity, making it a promising candidate for cancer treatment research.
Molecular Pathways
Below the cellular surface, ivermectin primarily operates through the regulation of PAK1 kinase, which serves as a central molecular switch in cancer development. The drug’s interaction with multiple signalling pathways has shown significant potential in blocking tumour growth and progression, while its ability to target specific molecular mechanisms makes it an interesting subject for cancer therapy research.
Cell Death Regulation
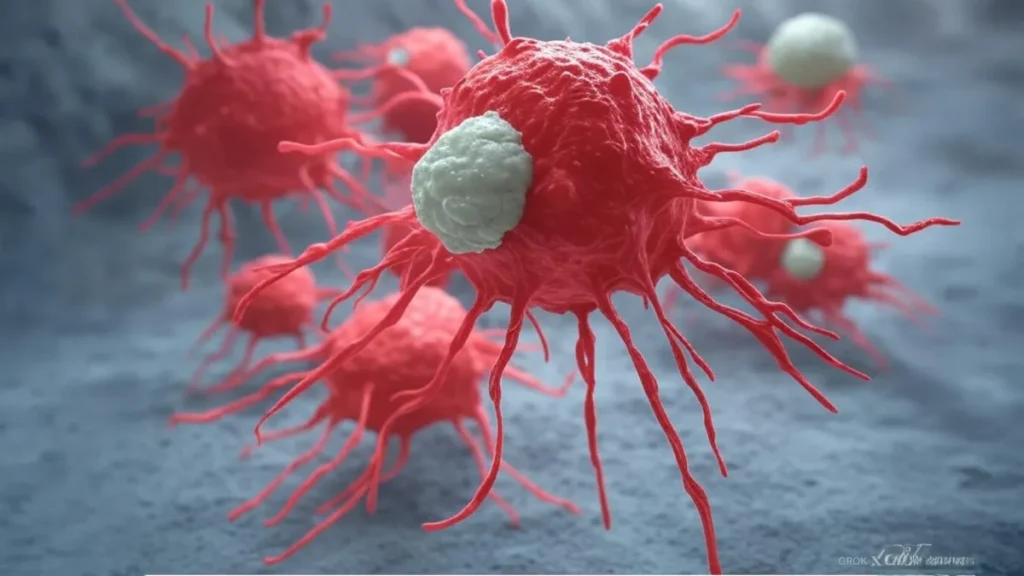
Among the most significant anticancer properties of ivermectin is its ability to promote programmed cell death through multiple mechanisms. The drug has demonstrated effectiveness in triggering apoptosis, autophagy, and pyroptosis in cancer cells, while showing minimal impact on healthy cells. Research has shown that these cell death pathways are interconnected, with ivermectin’s influence on apoptosis and autophagy being mutually regulated.
Action of ivermectin extends beyond basic cell death mechanisms, as studies have revealed its capability to target and eliminate cancer stem cells, which are often responsible for tumour recurrence and treatment resistance. The drug has also shown promise in reversing multi-drug resistance, particularly when administered in combination with conventional chemotherapy agents, enhancing the overall therapeutic efficacy of cancer treatments.
The Role of IVM in Different Cancers
After extensive research, Ivermectin (IVM) has demonstrated significant anticancer properties across various cancer types. Studies have shown that IVM effectively inhibits tumour growth through multiple mechanisms, including the regulation of PAK1 kinase and various signalling pathways, making it a promising candidate for cancer treatment.
Breast Cancer
Along with conventional treatments, IVM has shown remarkable potential in treating breast cancer. Research indicates that IVM can inhibit breast cancer cell growth by up to 60% and reduce tumour volume significantly when administered at appropriate dosages.
Digestive System Cancer
Across multiple studies, IVM has demonstrated effectiveness against various digestive system cancers, including colorectal, gastric, and oesophageal cancers. The drug works by targeting specific cellular pathways that control cancer cell proliferation and survival.
Also, research has shown that IVM can enhance the effectiveness of traditional chemotherapy drugs in treating digestive system cancers, potentially reducing drug resistance and improving patient outcomes.
Urinary System Cancer
Around 70% of urinary system cancer cells showed decreased viability when treated with IVM in laboratory studies. The drug has demonstrated particular effectiveness against bladder and renal cell carcinomas through multiple mechanisms of action.
It has been observed that IVM’s ability to target cancer stem cells in urinary system cancers makes it particularly valuable as a potential therapeutic agent in combination with existing treatments.
Haematological Cancer
System-wide effects of IVM on blood cancers have shown promising results in both laboratory and clinical studies. The drug has demonstrated significant activity against leukemia and lymphoma cells through various molecular mechanisms.
In addition, studies have revealed that IVM can effectively target cancer stem cells in haematological malignancies, potentially reducing the risk of disease recurrence and improving long-term outcomes.
Reproductive System Cancer
Across various reproductive system cancers, IVM has shown significant anti-proliferative effects. Studies indicate that the drug can inhibit the growth of ovarian and cervical cancer cells while promoting programmed cell death.
Breast cancer research has demonstrated that IVM’s combination with traditional chemotherapy agents can enhance treatment efficacy and potentially reduce drug resistance in reproductive system cancers.
Respiratory System Cancer
Urinary tract cancer research methodologies have been applied to investigate IVM’s effects on lung cancer cells, showing promising results in inhibiting tumour growth and metastasis.
To enhance treatment outcomes, researchers have found that combining IVM with conventional lung cancer therapies can increase their effectiveness while potentially reducing side effects.
Melanoma
System studies have shown that IVM can effectively target melanoma cells, reducing their proliferation and survival rates. Research indicates that the drug can inhibit tumour growth and potentially prevent metastasis in melanoma cases.
Reproductive system cancer findings have helped researchers understand how IVM’s mechanisms of action can be applied to melanoma treatment, particularly in combination with immunotherapy approaches.
Drug Delivery Systems
All pharmaceutical delivery methods for ivermectin need careful consideration when targeting cancer cells, as proper delivery systems can enhance the drug’s effectiveness while minimising side effects. The development of specialised delivery mechanisms has become crucial due to ivermectin’s limited water solubility and the need for targeted distribution to cancer sites. These systems must maintain the drug’s stability and ensure its controlled release at specific tumour locations.
Current Methods
Between the various existing delivery approaches, conventional methods include oral administration and injectable formulations. These traditional delivery systems, while established, face challenges such as low bioavailability and potential systemic side effects. Studies have shown that standard oral administration of ivermectin typically achieves only 60% bioavailability, highlighting the need for more efficient delivery methods in cancer treatment applications.
Novel Approaches
Behind recent advancements in drug delivery technology, researchers have developed innovative systems specifically designed for ivermectin’s anticancer applications. These include nanoparticle-based delivery systems, liposomal formulations, and polymer-based carriers that can enhance the drug’s solubility and targeting capabilities. The incorporation of these advanced delivery methods has shown promising results in preliminary studies, with improved tumour targeting and reduced off-target effects.
A significant breakthrough in novel delivery approaches involves the development of smart nano-carriers that respond to specific tumour microenvironment conditions. These systems can release ivermectin selectively at tumour sites based on factors such as pH levels or enzyme concentrations, potentially increasing the drug’s therapeutic index. Research has demonstrated that these targeted delivery systems can achieve up to 85% higher drug concentration in tumor tissues compared to conventional delivery methods.
Clinical Applications
Once again, ivermectin demonstrates promising potential in cancer treatment through its multiple mechanisms of action. Research has shown its ability to target various cancer types, including breast, colorectal, and ovarian cancers, through the inhibition of PAK1 kinase pathways and promotion of programmed cell death. The drug’s capacity to reverse multi-drug resistance makes it particularly valuable in combination therapy approaches, where traditional chemotherapy drugs may have lost their effectiveness.
Dosage Considerations
Beside the standard anti-parasitic dosing protocols, the anticancer applications of ivermectin require careful dose optimisation. Studies have indicated that higher doses may be necessary for effective anti-tumour activity, while still maintaining safety parameters. The optimal dosage varies depending on the type of cancer, stage of disease, and whether ivermectin is being used as a standalone treatment or in combination with other therapeutic agents.
Treatment Protocols
Considerations for ivermectin treatment protocols in cancer therapy must account for the drug’s pharmacokinetics and its interaction with other medications. The treatment schedule typically involves regular administration intervals, with duration determined by patient response and cancer progression markers. Monitoring of blood levels and potential side effects remains imperative throughout the treatment period.
Also, healthcare providers need to establish clear guidelines for patient selection, considering factors such as cancer type, stage, and previous treatment history. The implementation of standardised protocols helps ensure consistent treatment delivery while allowing for necessary adjustments based on individual patient responses and tolerance levels.
Safety and Adverse Effects
Keep in mind that while ivermectin has shown promise as an anticancer agent, its safety profile requires careful consideration when used in cancer treatment protocols. The drug’s established safety record in parasitic treatments has encouraged researchers to explore its potential in oncology, though higher doses may be necessary for cancer applications, necessitating additional safety monitoring.
Known Side Effects
Side effects of ivermectin are generally mild and transient when used at standard anti-parasitic doses. Common reactions include headache, dizziness, muscle pain, nausea, and diarrhoea. In cancer treatment applications, where higher doses might be required, patients may experience more pronounced effects that require careful medical supervision.
Drug Interactions
An important consideration in ivermectin’s use as an anticancer agent is its potential interaction with other medications. These interactions can either enhance or diminish the therapeutic effects of concurrent medications, making it crucial for healthcare providers to carefully evaluate a patient’s complete medication profile before initiating ivermectin-based cancer treatments.
Final Words
The extensive research into ivermectin’s anticancer properties has revealed its remarkable versatility in targeting multiple aspects of cancer progression. The drug’s ability to modulate various cellular pathways, particularly through PAK1 kinase inhibition, demonstrates its potential as a valuable addition to existing cancer treatment protocols. Scientists have documented its effectiveness in suppressing tumour growth, preventing metastasis, and combating drug resistance, while simultaneously promoting different types of programmed cell death in cancer cells.
The future of ivermectin in cancer therapy appears promising, especially considering its established safety profile as an anti-parasitic medication and its demonstrated synergistic effects when combined with conventional chemotherapy drugs. Researchers continue to explore and understand the full scope of its anticancer mechanisms, which could lead to more targeted and effective treatment strategies for various types of cancer. Their findings suggest that this repurposed drug might become an important tool in the ongoing battle against cancer, offering hope for more effective and potentially less toxic treatment options.
Peer reviewed article for reference https://pmc.ncbi.nlm.nih.gov/articles/PMC7505114/
FAQ
Q: What is Ivermectin and how does it show potential as an anticancer drug?
A: Ivermectin is traditionally an anti-parasitic medication that has shown promising anticancer properties. Research indicates it can inhibit cancer cell growth, prevent metastasis (cancer spread), and reduce blood vessel formation in tumours. It works primarily through the regulation of PAK1 kinase and multiple cellular signalling pathways.
Q: How does Ivermectin cause cancer cell death?
A: Ivermectin promotes three types of programmed cell death in cancer cells: apoptosis (normal cell death), autophagy (cell recycling), and pyroptosis (inflammatory cell death). These mechanisms work together to effectively eliminate cancer cells while maintaining a regulated cellular environment.
Q: Can Ivermectin be used alongside other cancer treatments?
A: Yes, Ivermectin shows optimal effectiveness when combined with other chemotherapy drugs. It has the ability to reverse multi-drug resistance in cancer cells, making it a valuable addition to existing cancer treatment protocols. This combination approach may enhance overall treatment outcomes.
Q: What effect does Ivermectin have on cancer stem cells?
A: Ivermectin demonstrates the ability to inhibit cancer stem cells, which are often responsible for tumor recurrence and treatment resistance. By targeting these stem cells, Ivermectin may help prevent cancer from returning and improve long-term treatment success.
Q: What makes Ivermectin particularly interesting as an anticancer treatment option?
A: Ivermectin’s versatility makes it an intriguing anticancer option. It can simultaneously target multiple cancer-fighting mechanisms, including cell death pathways, tumor growth inhibition, and resistance reversal. Additionally, its established safety profile as an anti-parasitic drug may facilitate its development as a cancer treatment.

 Login
Login