What Everyone Gets Wrong About Recovery From Addiction
Misconceptions about recovery from addiction can lead to damaging misunderstandings that affect your journey. Many people believe that recovery is a linear process or a quick fix, but in reality, it often involves setbacks and considerable effort. It’s important to recognize that recovery is not just about stopping substance use; it encompasses emotional healing, acquiring new coping skills, and building a supportive community. By shedding these common myths, you can pave a more informed and constructive path toward your holistic healing.
Key Takeaways:
- Recovery is a personal journey, and there is no one-size-fits-all approach; each individual may require a different method to find success.
- Abstinence is just one aspect of recovery; addressing underlying mental health issues and emotional well-being is imperative for long-term healing.
- Support systems play a vital role in recovery; building strong relationships with family, friends, or support groups can enhance the recovery process.
- Relapse is often a part of the recovery journey and should not be viewed as a failure but rather as an opportunity for growth and reassessment.
- Stigma surrounding addiction can hinder recovery efforts; fostering understanding and compassion is important for individuals seeking help.
Understanding Addiction
For many, understanding addiction is the first step in overcoming misconceptions and fostering a more supportive environment for those in recovery. Addiction is a complex condition that extends beyond mere willpower or personal choice. It involves intricate interactions between genetics, brain chemistry, environmental factors, and emotional health. By grasping the multifaceted nature of addiction, you can develop a greater empathy not only for yourself but also for others grappling with this challenge.
The Nature of Addiction
The reality of addiction lies in its ability to hijack the brain’s reward system, altering how you feel pleasure and desire. This neurological change can result from repeated exposure to addictive substances or behaviors, often leaving you with an overwhelming compulsion to seek them out, despite the negative consequences. It’s vital to understand that addiction is not simply about poor choices; it’s a chronic disease that can require ongoing management and support, much like other health conditions.
Common Misconceptions
Nature often leads people to inaccurately view addiction as a moral failure or a sign of weakness. This misconception can perpetuate stigma and shame, making it even harder for you to seek help or for your loved ones to support you. The truth is, addiction can affect anyone, regardless of background, socioeconomic status, or personal values. Understanding that addiction can result from numerous factors empowers you to approach the situation with compassion rather than judgment.
Plus, many believe that overcoming addiction is a straightforward process—the idea that you can simply “decide” to stop and that will be the end of it. However, this belief dismisses the incredibly complex nature of addiction and ignores the need for professional help, support systems, and often a multi-faceted treatment approach. Recovery typically involves addressing both the physical and emotional aspects of addiction, making it pertinent for you to look at this journey as a long-term commitment rather than a quick fix.
The Recovery Process
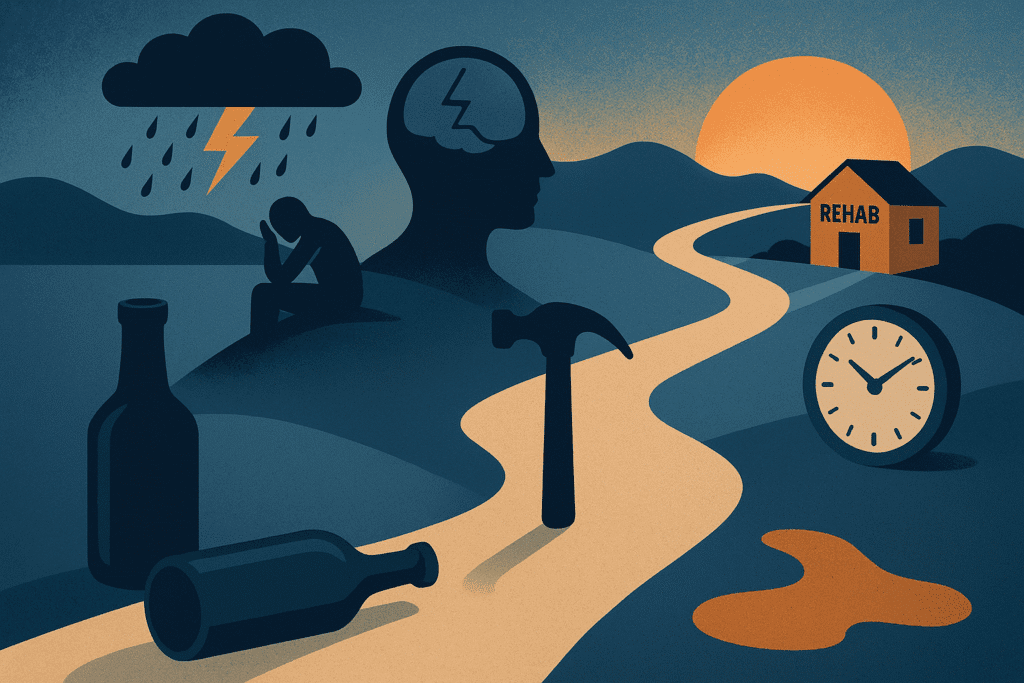
Clearly, the recovery process from addiction is not a one-size-fits-all journey. It involves various stages and levels of commitment that can vary greatly from one individual to another. Acknowledging that recovery is a non-linear path is crucial; it often entails ups and downs, making it paramount to be prepared for the challenges you may face along the way. Understanding that recovery requires time and effort is key to setting realistic expectations for yourself.
Stages of Recovery
Beside the common misconception that recovery is solely about abstaining from substance use, it’s crucial to grasp the distinct stages involved in this journey. These stages typically include precontemplation, contemplation, preparation, action, and maintenance. Each stage requires different levels of commitment and introspection, allowing you to understand where you stand and where you need to go. In precontemplation, you might not even recognize that you have a problem, while in action, you actively take steps to change your behavior.
Personalized Recovery Plans
Beside the stages of recovery, developing a personalized recovery plan is vital for your success. This plan should take into account your unique needs, triggers, and support systems. A one-size-fits-all program may not address the specific obstacles you face or the individual motivations that inspire you. Your recovery plan could include therapy, support groups, medication, or holistic approaches, tailored to ensure you have a strong foundation to build upon as you navigate through recovery.
Personalized recovery plans focus on your unique experiences and circumstances, emphasizing that there is no universal solution to addiction recovery. You’ll want to consider factors like your personal history, medical needs, and the specific triggers that led to your addiction in the first place. Involving professionals who can assist in crafting a plan that resonates with you can help you stay accountable and motivated. Your personalized plan should be adaptable; as you progress, revisiting and modifying it to reflect your changing needs ensures that you continually remain on the path toward a fulfilling, sober life.
Support Systems
Keep in mind that Recovery From Addiction is rarely a solo journey; instead, it often thrives on the foundation of a solid support system. You might assume that you can navigate this path alone, but that misconception can lead to setbacks and isolation. Surrounding yourself with individuals who genuinely care for your well-being, whether they are family members, friends, or fellow recovering addicts, can significantly enhance your chances of long-term success. It’s important to understand that these support networks provide not just emotional encouragement, but also practical advice and shared experiences that can guide you through the turbulent waters of recovery.
Role of Professional Help
Support systems are not solely composed of loved ones; integrating professional help into your recovery plan can be a game-changer. Engaging with trained therapists or counselors who specialize in addiction gives you access to valuable insights and coping mechanisms. These professionals can help you identify the underlying issues that may have contributed to your addiction and equip you with strategies to manage cravings and triggers. A structured treatment program often aligns your recovery with proven therapeutic models, offering a safe space to dive deeper into your recovery journey.
Importance of Community Support
Below the surface, community support plays a significant role in your recovery. Participating in group therapy sessions or local support groups not only offers moral support but also reinforces the belief that you are not alone in this fight. Listening to others share their stories and struggles can help you to recognize that recovery is a shared experience and that it is entirely normal to face challenges along the way. Sharing your own experiences allows you to process your journey, gains perspective, and may even inspire someone else.
Understanding the multifaceted nature of recovery means valuing the role played by community support systems. Engaging with others who have faced similar challenges can foster a sense of belonging and reduce feelings of shame and isolation. This shared experience enhances your ability to cope with stressors, as positive connections can bolster your resilience. Additionally, community support can serve as a powerful reminder that progress is possible and achievable, reinforcing your commitment to stay on the path of recovery and find strength through unity. Investing your time and energy in such connections can make all the difference in your journey towards a healthier, addiction-free life.
Relapse and Setbacks
Unlike what many may believe, relapse is not a failure but a common part of the recovery journey. Your path to sobriety can be fraught with challenges, and setbacks can occur, especially when facing triggers or stressful situations. Understanding that relapse can happen and does not mean you are weak or incapable is vital. In fact, many people in recovery experience multiple relapses before finding a lasting solution. What is important is how you respond to these moments and what you learn as you navigate your journey.
Understanding Relapse
Against the prevailing notion that a setback signals the end of your recovery, it is important to shift your perspective. A relapse can offer insights into vulnerabilities you may need to address or situations to avoid in the future. Contemplating the factors that led to your setback can provide valuable lessons that strengthen your long-term resilience. By dissecting the circumstances surrounding your relapse, you can develop a more robust preventive strategy for the future.
Strategies for Overcoming Setbacks
After experiencing a setback, it’s important to refocus your efforts and implement effective strategies that can guide you toward a successful recovery. Acknowledging your feelings and fearlessly exploring the emotions tied to your relapse can help you process the experience rather than bury it. Develop a well-rounded support system of peers, counselors, and family who can provide encouragement and accountability. Additionally, practicing mindfulness techniques, such as journaling or meditation, can help you regain clarity and stability in your recovery journey.
Understanding the importance of proactive coping mechanisms can reshape how you approach future challenges. Building a personal toolbox filled with resources like sober activities, relaxation techniques, and accountability partners can significantly aid in managing cravings and avoiding triggers. By being prepared and equipping yourself with positive strategies, you can face setbacks with greater confidence and resilience, ultimately paving the way for a stronger path to recovery.
Long-Term Recovery
Your journey towards long-term recovery from addiction involves more than just abstaining from substance use; it requires an intentional approach to building a healthy lifestyle. The process is deeply rooted in creating and maintaining healthy habits that support your mental, emotional, and physical well-being. These habits may include regular exercise, balanced nutrition, and sufficient sleep. Incorporating activities that promote self-care, such as mindfulness practices and hobbies, can also play a significant role in fostering resilience against triggers that may lead to relapse. The key is consistency—by embedding these healthy practices into your daily routine, you begin to reshape your life and environment in ways that nurture growth and stability.
Building Healthy Habits
By understanding that recovery is a long-term commitment, you will recognize the importance of building healthy habits that reinforce your sobriety. This includes not just the elimination of harmful substances, but also the adoption of positive behaviors that enhance your quality of life. For instance, establishing a routine can provide structure, while social connections can offer invaluable support. Engaging in physical activities or creative pursuits can act as effective outlets for stress and emotions that may arise during your recovery journey. Focus on setting small, achievable goals that allow you to celebrate your progress, further motivating you to continue on this healthy path.
Emphasizing Lifestyle Changes
Changes to your lifestyle play a significant role in maintaining recovery, as they help reshape your daily experiences and environments. This can mean distancing yourself from places and people that trigger cravings or revisiting certain social circles that prioritize sobriety. Surrounding yourself with a supportive community, whether through recovery groups or new friendships, involves a fundamental lifestyle shift that promotes accountability and emotional support. Lifestyle changes may also encompass daily rituals such as practicing gratitude, volunteering, or participating in community events—activities that deepen your connection with others and foster a sense of purpose.
Understanding how lifestyle changes affect your recovery enhances your ability to stay focused on your goals. It involves examining your daily routines and identifying areas where you can replace negative influences with constructive actions. Building a healthier social network, adopting stress-reduction techniques, and prioritizing self-care can all provide protective factors against relapse. Committing to these shifts not only supports your long-term sobriety but also enriches your overall quality of life, enabling you to thrive beyond addiction.
Myths vs. Facts
To effectively navigate the intricate path of recovery from addiction, it’s vital to separate fact from fiction. Misunderstandings abound, creating barriers that can hinder your progress and perpetuate stigma. Many individuals believe that recovery is simply about willpower or that it can be achieved within a fixed timeframe. These myths can lead to feelings of failure or inadequacy when, in reality, recovery is a unique journey that varies person to person. You need to recognize that while the process may seem overwhelming, acknowledging and addressing these myths can bolster your understanding and commitment to your recovery journey.
Debunking Common Myths
Debunking common myths surrounding addiction recovery allows you to grasp the reality of your situation. For instance, it is a widespread belief that addiction is a moral failing rather than a chronic disease. This misconception can instill a sense of shame, making it harder for you to seek help or ask for support. Additionally, many think that once you complete a treatment program, recovery is a one-time event, rather than an ongoing process that involves continuous growth and potential setbacks. The truth is, recognizing recovery as a lifelong commitment encourages you to embrace setbacks as part of your process rather than failures.
Evidence-Based Recovery Approaches
Facts about recovery emphasize the importance of utilizing evidence-based approaches, which are proven to be effective in promoting long-term success. These methods, such as cognitive-behavioral therapy (CBT) and motivational interviewing, are supported by scientific research and provide you with the necessary tools and strategies to address both the psychological and emotional aspects of substance use. When you engage in these evidence-based practices, you are not just relying on anecdotal experiences; you are participating in a system backed by substantial evidence, fostering a more informed recovery journey.
The integration of evidence-based recovery approaches into your journey underscores the significance of tailored treatment options. Programs that employ evidence-based methods boast higher success rates due to their focus on individualized needs and challenges. By participating in therapies that have been rigorously tested and shown to aid in recovery, you empower yourself with knowledge and techniques that can significantly enhance your chances of maintaining sobriety. This proactive approach not only boosts your skills in managing cravings and triggers but also equips you with a support system that is rooted in understanding and results.
Conclusion
Hence, understanding recovery from addiction requires a comprehensive perspective that goes beyond common misconceptions. You might be led to believe that recovery is a linear journey, marked by clear milestones and a straightforward path to sobriety. In reality, recovery encompasses a complex interplay of emotional, mental, and social factors, making it vital to accept that setbacks may occur and are a natural part of your journey. By recognizing the multifaceted nature of recovery, you empower yourself to navigate the challenges ahead with resilience and a more informed mindset.
Additionally, you may find that the societal stigma surrounding addiction can make your struggle feel isolating. It’s vital to acknowledge that addiction is a health issue rather than a personal failing, and seeking help is a strength, not a weakness. Embrace the idea that recovery is possible with the right support system, coping mechanisms, and treatment options. By breaking down the misconceptions you encounter, you pave the way for a more constructive and empathetic approach to your healing process, aligning your recovery goals with the reality of what it takes to achieve a healthier, fulfilling life.
Meducate has a great introductory webinar called What is Addiction and is free
Q: What is a common misconception about the timeline of recovery from addiction?
A: Many people believe that recovery from addiction follows a linear path and can be completed within a certain amount of time. In reality, recovery is a highly individual process that varies from person to person. Factors such as the severity of the addiction, personal circumstances, and individual mental health can all influence the length and trajectory of recovery. Some individuals may experience setbacks or relapses along the way, but these should not be seen as failures; they are often part of the complex journey towards sustained sobriety.
Q: Do people often underestimate the importance of ongoing support in the recovery process?
A: Yes, a prevalent misunderstanding is that once someone completes a treatment program, they are fully recovered and need no additional support. In truth, continuing support is vital for long-term recovery. This can include participation in support groups, therapy, and maintaining connections with sober friends and family. Ongoing support helps individuals cope with the challenges of everyday life, reinforces positive habits, and provides encouragement during difficult times.
Q: What role do co-occurring mental health issues play in recovery that people might overlook?
A: Many individuals do not recognize how common it is for addiction to co-exist with mental health disorders such as depression, anxiety, or PTSD. Ignoring these co-occurring issues can complicate the recovery process. Successful recovery often requires an integrated approach that addresses both addiction and mental health simultaneously. By treating both the substance use and any underlying mental health conditions, individuals are more likely to achieve lasting recovery.